Non-invasive examinations or challenge tests represent a valuable complementary option
The degree of the inflammation so far has been determined primarily via samples collected from patients’ airways or lungs. To this end, either coughing was induced for sputum collection (induced sputum) or bronchoscopy was performed to collect cells from the lungs by means of brush biopsies or lung lavage. Performance of these examinations can be perfectly safe and they provide important information about the cellular composition and cell activation status in the airways and lungs; however, they also put a certain strain on study participants, so that methods involving no invasive examinations or challenge tests for sample collection represent a valuable complementary option for efficacy testing of pharmaceuticals.
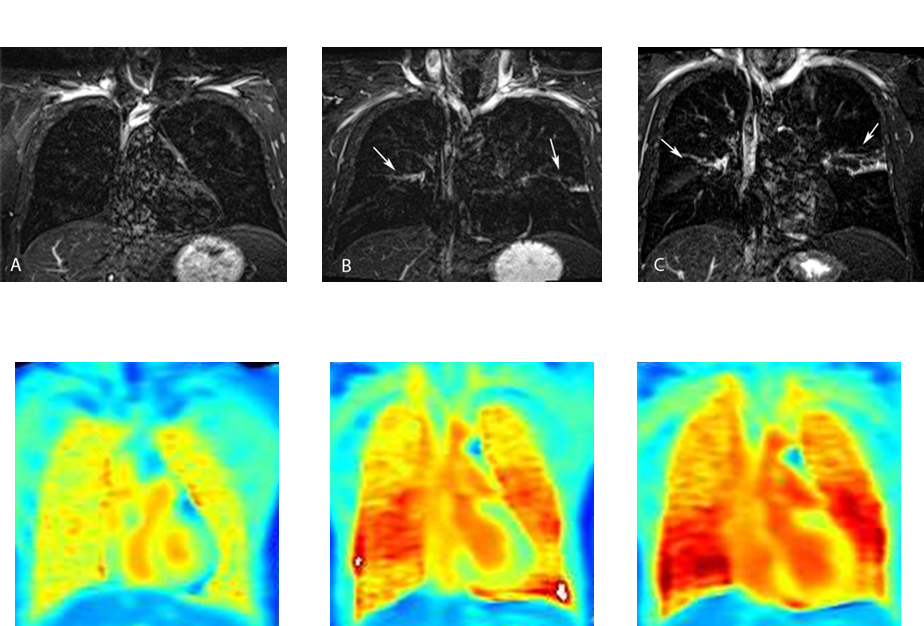
Magnetic resonance imaging (MRI) is one such non-invasive method, used to generate images of the human lung. The aim of current research activities is to improve the imaging technology, so as to enable visualization not only of the lung’s structure, but also of inflammatory processes. Airway inflammation involves an influx of liquid into the lung tissue, reduced local ventilation and blood flow, and diminished gas exchange in the lung tissue. By further development of the traditional MRI technology, diagnostic imaging of these processes is possible with magnetic resonance imaging methods. In addition to the classical proton-based sequences, functional examination sequences are used in particular. Furthermore, methods are being developed that enable contrast enhancement in the lungs by means of a gaseous contrast agent, instead of using the traditional proton-based MRI technology.
 Fraunhofer Institute for Toxicology and Experimental Medicine
Fraunhofer Institute for Toxicology and Experimental Medicine